What Is This Herd Immunity?
Three times in the last year I have heard the term “Herd Immunity.” The first was during my physical, in the history taking portion. The second time was during treatment of a minor eye infection. The third was in an article I was studying for continuing education in occupational health.
The rather odd sounding phrase prompted a little intellectual curiosity. “What is this herd immunity?”
“Herd Immunity; A Rough Guide” lists three uses for the term “herd immunity.” Used to:
- Describe the portion of “immune” individuals within a population.
- Threshold portion of immune individuals that should lead to a decline in incidence of infection.
- Risk of infection among susceptible individuals in a population is reduced by the presence and proximity of immune individuals.
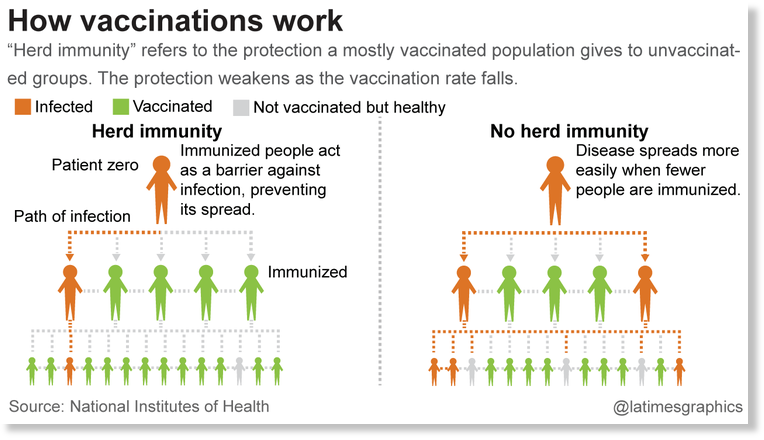
As I understand it, the basic theory of “herd immunity” is this: the incidence of a disease decreases over time because more people are immune to the disease. If a large percentage of the population is immune to a disease, the risk of transmitting the disease declines because less people are becoming sick. The cycle of disease transmission is theoretically broken.
Vaccination programs obviously provide an important element in the battle against the spread of communicable disease. The subject gets complex as more people elect to forgo immunizations, or have never had the opportunity for vaccinations.
I found this reference to a CDC (Centers for Disease Control and Prevention) report in a “Health Day” article listing the percentage of adults in the general population that have received vaccinations for specific diseases. The adult/vaccination rates included:
- Pneumonia: Overall, 20 percent of high-risk adults received this vaccination in 2012, about the same number as in 2011. Among adults 65 and older, 60 percent were vaccinated overall.
- Tetanus: About 64 percent of adults aged 19 to 64 received some tetanus-containing vaccine in the previous 10 years -- about the same as the previous year.
- Tdap: Coverage against diphtheria, pertussis and tetanus increased modestly to nearly 16 percent, but in homes with infants under 1 year, coverage was almost 26 percent, similar to the prior year.
- Hepatitis A: Only 12 percent of adults aged 19 to 49 had full hepatitis A vaccination coverage (at least two doses) in 2012.
- Hepatitis B: About 35 percent of U.S. adults aged 19 to 49 had the recommended three or more doses of hepatitis B vaccine, much the same as in 2011.
- Herpes Zoster: Twenty percent of adults age 60 and older received this vaccine to protect against shingles, up from fewer than 16 percent in 2011.
- HPV: Almost 35 percent of women aged 19 to 26 received one or more doses of this vaccine, which protects against cervical cancer, up from about 30 percent the year before. About 2 percent of males in this age group got the vaccine, similar to the 2011 number.
What’s the implication for businesses? Sick workers can’t work. An outbreak of some of the diseases listed above can spread rapidly through a largely unprotected work force. Healthcare workers and other employees with direct contact with the very young, elderly and critically sick persons can have a dramatic impact on outcomes.
Are your workers aware of the health effects of some of these diseases? Are workers making use of medical resources available to them? Have vaccines been included in the medical benefits package? What’s your immunological status?
This CDC Quiz can be a tool to help an adult determine what vaccines are recommended based upon one’s answers.